Understanding Sleep Apnea

Sleep apnea, a sleep disorder characterized by interruptions in breathing during sleep, presents a significant hurdle to restorative rest. This condition disrupts the natural sleep cycle, affecting both physical health and overall well-being. To delve deeper into this prevalent disorder, it’s crucial to explore its types, common causes, associated risks, and potential avenues for management.
Types of Sleep Apnea
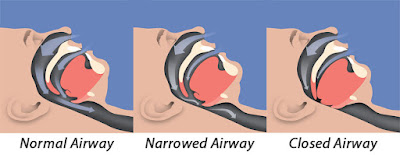
1. Obstructive Sleep Apnea (OSA)
OSA, the most common form, occurs when the throat muscles relax, causing the airway to narrow or close during sleep. This obstruction leads to breathing pauses, often accompanied by loud snoring.

2. Central Sleep Apnea (CSA)
CSA results from a lack of effort in breathing due to the brain's failure to send proper signals to the muscles responsible for respiration during sleep. Unlike OSA, there's no physical obstruction in the airway.
3. Mixed Sleep Apnea
This type combines features of both obstructive and central sleep apnea, presenting challenges in diagnosis and treatment.

Common Causes of Sleep Apnea
1. Physical Factors
- Obesity: Excessive weight can contribute to OSA by increasing soft tissue around the neck, and narrowing the airway.
- Narrow Airway: Genetics or enlarged tonsils/adenoids may lead to a smaller airway, predisposing individuals to obstructive sleep apnea.
- Age and Gender: Middle-aged and older adults, as well as males, are at higher risk.
2. Lifestyle Factors
- Alcohol and Sedatives: These substances relax throat muscles, exacerbating OSA symptoms.
- Smoking: Smoking can increase inflammation and fluid retention in the upper airway.
3. Medical Conditions
- Hypertension and Heart Conditions: Sleep apnea is often associated with cardiovascular issues due to the strain on the heart caused by interrupted breathing during sleep.
- Neurological Disorders: Conditions like Parkinson's disease or stroke can affect the brain's respiratory control, leading to central sleep apnea.

Risk Factors Associated with Sleep Apnea
1. Family History:
A family history of sleep apnea increases the likelihood of its development.
- Age and Gender: As mentioned earlier, older adults and males are at higher risk.
- Ethnicity: Certain ethnic groups are more prone to sleep apnea.
- Medical Conditions: Pre-existing medical conditions like diabetes or nasal congestion can elevate the risk.
- Smoking and Alcohol Use: Lifestyle choices contribute significantly to the risk profile.
Impact on Health and Daily Life
The consequences of untreated sleep apnea extend beyond sleep disturbances, encompassing a spectrum of health issues:
- Daytime Fatigue: Interrupted sleep leads to daytime sleepiness, affecting concentration and productivity.
- Cardiovascular Problems: Hypertension, heart disease, and strokes are linked to untreated sleep apnea.
- Mental Health: Increased risk of depression, anxiety, and irritability due to poor sleep quality.
- Metabolic Issues: Weight gain, insulin resistance, and diabetes are correlated with sleep apnea.
Seeking Diagnosis and Treatment
Identifying sleep apnea involves assessments such as sleep studies, where breathing patterns and disruptions are monitored overnight. Treatment options depend on the severity and type of sleep apnea:

Continuous Positive Airway Pressure (CPAP):
A common treatment involves a machine that delivers a steady stream of air through a mask, keeping the airway open during sleep.
- Oral Appliances: Dental devices reposition the jaw to prevent airway obstruction.
- Surgery: In severe cases, surgical procedures may be recommended to address anatomical issues causing obstruction.
- Lifestyle Changes: Weight loss, quitting smoking, and avoiding alcohol can significantly improve symptoms.
Can You Fix Sleep Apnea?
While sleep apnea may not always be completely "fixed," it can be effectively managed, significantly improving symptoms and reducing associated risks. Treatment aims to minimize interruptions in breathing during sleep and alleviate symptoms to promote restful sleep and improve overall health.
What Worsens Sleep Apnea?
1. Obesity:
Excessive weight can lead to increased fat deposits around the neck, narrowing the airway and worsening obstructive sleep apnea.
2. Alcohol and Sedatives:
Consuming alcohol or sedatives relaxes the throat muscles, contributing to airway obstruction during sleep.
3. Smoking:
Smoking causes inflammation and fluid retention in the upper airway, exacerbating sleep apnea symptoms.
4. Nasal Congestion:
Allergies or sinus issues causing nasal congestion can obstruct airflow, aggravating sleep apnea.
5. Sleeping Position:
Sleeping on the back may allow the tongue and soft tissues to collapse into the airway, leading to breathing difficulties.
6. Untreated Medical Conditions:
Conditions such as hypertension, heart disease, or diabetes can worsen sleep apnea and vice versa, forming a complex interplay between health issues.
Addressing these contributing factors through lifestyle changes and adhering to prescribed treatments can significantly improve sleep apnea symptoms and overall quality of sleep. Seeking guidance from healthcare professionals for tailored treatment strategies is essential for effective management.
Conclusion: Navigating the Path to Better Sleep
Sleep apnea, a multifaceted condition, demands attention and proactive management. Understanding its types, recognizing common causes and risks, and seeking timely diagnosis and appropriate treatment empower individuals to reclaim restful nights and pave the way for better health and vitality. Consultation with healthcare professionals remains pivotal in the journey toward mitigating the impacts of sleep apnea and achieving a rejuvenating night's sleep.
